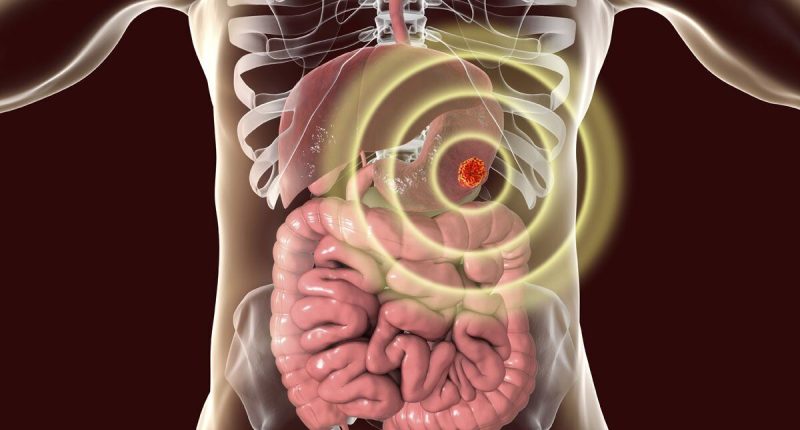
Cancer: Risk Factors For Colon Cancer May Include Shellfish Intake – Cancer is caused by mutations in the DNA cells that spur out of control and eventually grow into tumours. Left untreated, the condition can continue to invade the body’s tissue until it becomes untreatable. Several dietary sources, including shellfish, have been recognized as significant risk factors for the disease.
A study titled “Shellfish consumption: a major risk factor for colorectal cancer” in the Journal of Medical Hypotheses in 2008 highlighted the potential carcinogenic effects of eating certain shellfish.
What are the main risk factors for colon cancer?
Your risk of getting colorectal cancer increases as you get older. Other risk factors include having.
- Inflammatory bowel disease such as Crohn’s disease or ulcerative colitis.
- A personal or family history of colorectal cancer or colorectal polyps.
- A genetic syndrome such as familial adenomatous polyposis (FAP)external icon or hereditary non-polyposis colorectal cancer (Lynch syndrome).
The report warned that specific toxins that trigger a gastrointestinal illness may subsequently lead to the development of digestive cancer.
The researchers cautioned: “Sometimes, shellfish accumulates diarrhetic shellfish poisoning (DSP) toxins, which prove a gastrointestinal illness.”
Biotin is a type of naturally occurring microscopic algae eaten by shellfish. Once consumed, the crustaceans retain the toxin.

People can quickly become ill from eating shellfish contaminated with DPS.
Within 30 minutes to a few hours, a person may expect diarrhoea, nausea, vomiting and abdominal pain which may take three days to recover from.
“Furthermore,” continued the authors, “DSP toxins are tumour promoters that could increase colorectal cancer risk”.
“The current regulation about the level of DSP toxins in shellfish meat is only centred on reduction of the gastrointestinal symptoms.
“Unfortunately, legal level of DSP toxins in shellfish are enough to increase colorectal cancer risk.”
The findings were later echoed in a 2013 study published in Marine Drugs, which highlighted the need for further research on humans.
They said: “Tumour-promoting, mutagenic and immunosuppressive effects shown in animals to be associated with DST have not been confirmed in humans.
“However, several studies suggest that chronic exposure may increase the risk of gastrointestinal cancers.”
Cancer: Risk Factors For Colon Cancer May Include Shellfish Intake
What’s more, cancer prevention recommendations that are based on strong evidence do not include eating fish because the evidence is not yet strong, according to Cancer Council.
“However, because of the overall health benefits of fish and omega-3 fats, Cancer Council recommends eating fish (preferably oily) at least twice per week,” adds the body.
In fact, fats have been found in several studies to be associated with a reduced risk of breast cancer and its recurrence.
Some shellfish too, notably oysters and cockles, contain high amounts of iron and protein that promote a healthy brain, heart and immune system.
What Are the Symptoms of Colorectal Cancer?
Colorectal polyps (abnormal growths in the colon or rectum that can turn into cancer if not removed) and colorectal cancer don’t always cause symptoms, especially at first. Someone could have polyps or colorectal cancer and not know it. That is why getting screened regularly for colorectal cancer is so important.
If you have symptoms, they may include—
- A change in bowel habits.
- Blood in or on your stool (bowel movement).
- Diarrhea, constipation, or feeling that the bowel does not empty all the way.
- Abdominal pain, aches, or cramps that don’t go away.
- Weight loss and you don’t know why.
If you have any of these symptoms, talk to your doctor. They may be caused by something other than cancer. The only way to know what is causing them is to see your doctor.
What Is Colorectal Cancer Screening?
A screening test is used to look for a disease when a person doesn’t have symptoms. (When a person has symptoms, diagnostic tests are used to find out the cause of the symptoms.)
Colorectal cancer almost always develops from precancerous polyps (abnormal growths) in the colon or rectum. Screening tests can find precancerous polyps, so that they can be removed before they turn into cancer. Screening tests can also find colorectal cancer early, when treatment works best.
Screening Recommendations
Regular screening, beginning at age 45, is the key to preventing colorectal cancer and finding it early. The U.S. Preventive Services Task Force (Task Force) recommendsexternal icon that adults age 45 to 75 be screened for colorectal cancer. The Task Force recommends that adults age 76 to 85 talk to their doctor about screening.
The Task Force recommends several colorectal cancer screening strategies, including stool tests, flexible sigmoidoscopy, colonoscopy, and CT colonography (virtual colonoscopy). Learn about these screening tests.
When Should I Begin to Get Screened?
Most people should begin screening for colorectal cancer soon after turning 45, then continue getting screened at regular intervals. However, you may need to be tested earlier than 45, or more often than other people, if you have—
- Inflammatory bowel disease such as Crohn’s disease or ulcerative colitis.
- A personal or family history of colorectal cancer or colorectal polyps.
- A genetic syndrome such as familial adenomatous polyposis (FAP)external icon or hereditary non-polyposis colorectal cancer (Lynch syndrome).
If you think you are at increased risk for colorectal cancer, speak with your doctor about—
- When to begin screening.
- Which test is right for you.
- How often to get tested.
Post source: <a”> Daily Express </a”>