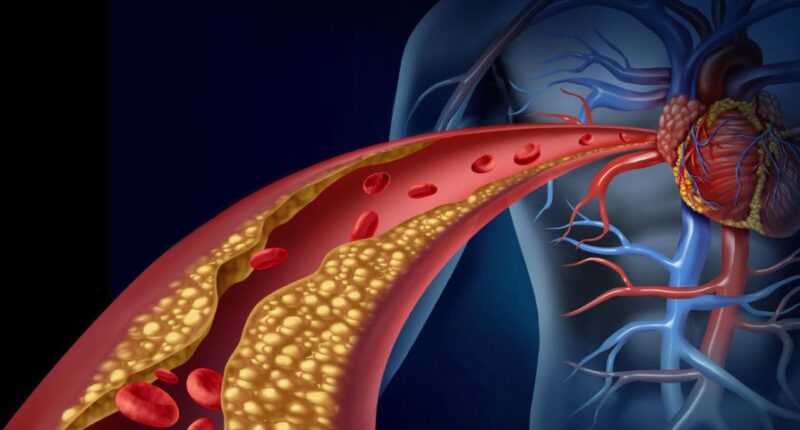
Diabetic dyslipidemia is a complex metabolic disorder that often accompanies diabetes mellitus. It involves an abnormal lipid profile, which can significantly increase the risk of cardiovascular disease. Understanding the symptoms, risk factors, and preventive measures associated with diabetic dyslipidemia is crucial for managing this condition effectively. In this comprehensive article, we will explore the intricacies of diabetic dyslipidemia symptoms, delve into the key risk factors, and discuss essential prevention strategies.
Diabetic Dyslipidemia Symptoms
Diabetic dyslipidemia, while often asymptomatic, can manifest in subtle ways. Recognizing these symptoms is vital for early detection and intervention:
- Xanthomas: These are fatty deposits that appear as yellowish lumps under the skin, typically around joints or tendons. Xanthomas can be indicative of elevated cholesterol levels, a common feature of diabetic dyslipidemia.
- Xanthelasma: Similar to xanthomas, xanthelasma manifests as yellowish patches on the eyelids. These patches are a potential sign of lipid imbalances and may be associated with diabetic dyslipidemia.
- Pancreatic Fat Accumulation: In some cases, diabetic dyslipidemia can lead to the accumulation of fat in the pancreas, impairing its function. This can exacerbate diabetes symptoms and complicate blood sugar management.
- Corneal Arcus: A white or grayish ring around the cornea of the eye, known as corneal arcus, can be a sign of elevated cholesterol levels, which are often seen in individuals with diabetic dyslipidemia.
- Eruptive Xanthomas: These are small, reddish-yellow bumps that may appear on the skin, often accompanied by itching. Eruptive xanthomas can signal severe lipid abnormalities.
Risk Factors for Diabetic Dyslipidemia
Understanding the risk factors associated with diabetic dyslipidemia is essential for assessing your susceptibility to this condition. Here are the key risk factors:
- Type 2 Diabetes: Individuals with type 2 diabetes are at a higher risk of developing diabetic dyslipidemia due to insulin resistance and impaired glucose metabolism.
- Genetics: A family history of lipid disorders can increase the likelihood of diabetic dyslipidemia. Genetic factors play a significant role in lipid metabolism.
- Obesity: Excess body fat, especially abdominal adiposity, is closely linked to dyslipidemia. Obesity can disrupt lipid homeostasis and exacerbate lipid abnormalities in diabetes.
- Poor Diet: Consuming a diet high in saturated and trans fats can contribute to dyslipidemia. These fats can elevate LDL cholesterol levels and lower HDL cholesterol, a common pattern in diabetic dyslipidemia.
- Physical Inactivity: A sedentary lifestyle can lead to weight gain and worsen insulin resistance, both of which are risk factors for diabetic dyslipidemia.
- Smoking: Smoking is detrimental to cardiovascular health and can exacerbate lipid abnormalities, increasing the risk of diabetic dyslipidemia-related complications.
- Age and Gender: As individuals age, the risk of diabetic dyslipidemia tends to increase. Men are also more likely to develop this condition than women.
Preventive Measures
Preventing or managing diabetic dyslipidemia is essential for reducing the risk of cardiovascular disease and complications associated with diabetes. Here are some effective preventive measures:
1. Glycemic Control
Achieving and maintaining good blood sugar control is paramount. This involves regular monitoring, adherence to prescribed medications or insulin therapy, and adopting a suitable dietary plan to manage blood glucose levels effectively.
2. Dietary Modifications
A heart-healthy diet plays a crucial role in managing diabetic dyslipidemia. Focus on:
- Reducing Saturated and Trans Fats: Limit the intake of foods high in saturated and trans fats, such as red meat, fried foods, and processed snacks.
- Increasing Fiber: Incorporate high-fiber foods like fruits, vegetables, and whole grains into your diet to help lower LDL cholesterol levels.
- Omega-3 Fatty Acids: Consume sources of omega-3 fatty acids, such as fatty fish (e.g., salmon and mackerel), flaxseeds, and walnuts, which can benefit heart health.
3. Regular Physical Activity
Engaging in regular exercise improves insulin sensitivity, helps manage body weight, and positively influences lipid profiles. Aim for at least 150 minutes of moderate-intensity aerobic activity per week.
4. Medications
In some cases, medications may be necessary to manage diabetic dyslipidemia effectively. Statins, fibrates, and other lipid-lowering drugs may be prescribed by a healthcare provider.
5. Smoking Cessation
If you smoke, quitting is imperative. Smoking cessation can lead to improvements in both lipid profiles and overall cardiovascular health.
6. Weight Management
Achieving and maintaining a healthy weight through a combination of diet and exercise can help improve lipid profiles and reduce the risk of diabetic dyslipidemia.
7. Regular Check-ups
Frequent medical check-ups are essential for monitoring lipid profiles and assessing cardiovascular risk. Regular screenings enable early detection and timely intervention.
8. Stress Management
Chronic stress can contribute to dyslipidemia. Adopt stress-reduction techniques such as mindfulness, yoga, or meditation to promote emotional well-being.
Conclusion
Diabetic dyslipidemia is a complex condition that requires careful management to mitigate its impact on cardiovascular health. Understanding the symptoms, recognizing the risk factors, and implementing preventive measures are crucial steps in effectively managing this condition. By adopting a holistic approach to diabetes and lipid profile management, individuals can reduce their risk of cardiovascular disease and lead healthier lives. Regular consultation with healthcare professionals is essential for personalized guidance and treatment tailored to individual needs.
Also Read | Does High Testosterone Cause Hair Loss in Females? Uncovering the Truth Behind Baldness
Last Updated on September 24, 2023 by 247 News Around The World